Historically, the language used in family conversations about organ and tissue donation has been thoroughly analyzed. After all, the way this conversation unfolds greatly impacts a family’s willingness to say “yes” to donation. On the other hand, the language used by OPO Hospital Development (HD) staff to lead and inspire our healthcare partners and influence changes in practice has not received the same analysis or attention.
HD Coordinators typically possess excellent written and verbal skills, an ability to cultivate and nurture effective relationships, and a knack for aligning those relationships with hospital systems to implement strategic initiatives that will optimize a hospital’s donation outcomes. All of this takes leadership.
Stephen Covey, best known for the book ‘Seven Habits of Highly Effective People’, suggests a leadership style that fits the work of HD perfectly: Principle-Centered Leadership.
But before we explore this leadership style, let’s take a look at two commonly utilized models, coercive power and utility power.
Coercive and utility power

Coercive power is largely based on fear and intimidation. The changes effected by leadership rely on the use of power and status, and often result in someone doing something out of fear. The follower may be left feeling leveraged and certainly uninspired. The follower “goes along to get along.”
Utility power is based on fairness and equity, and constitutes most working relationships. Leadership relies on fairness in an exchange between two parties, each of whom has something of value to the other. The changes effected in this model are based on someone doing something because it’s worth their while. It’s based on an exchange of support: “I support your issue, you support mine.”
Principle-centered leadership
Principle-centered leadership is about inspiring others to buy in and support a greater purpose and is based on mutual respect and trust. We all know that trust is fragile and takes a long time to develop. Many of us in the OPO community feel time is the enemy, especially for those we serve; transplant candidates on a waiting list. Time is also the enemy of HD Coordinators because the donation process must go right every time, all of the time, and the sooner a HD Coordinator can influence a more optimal process, the more likely it will go well the next time. It’s our job to fix broken or compromised processes and conduct immediate case follow up.
The major benefit of implementing a principle-centered leadership approach is that individuals perceive their leaders as honorable. Trust is established, and there’s a sense of feeling inspired. One’s ability to influence a better process and outcome must be connected to a larger purpose, and done so in an honorable and inspirational way.
When working with hospital partners, we must not only seek their input but, even more important, we must seek to educate ourselves and understand the reasons behind what they’re saying and how they’re feeling. Listening in an empathetic way can be an effective approach to strengthening relationships of trust and discovering more about the perspectives and feelings of our healthcare partners who care for critically ill patients and families. Failing to identify their perspectives or refusing to acknowledge them could have a detrimental and long-term impact on relationships, the process, and outcomes.
What’s your style?
Take a minute and evaluate your own leadership style by considering the following statements:
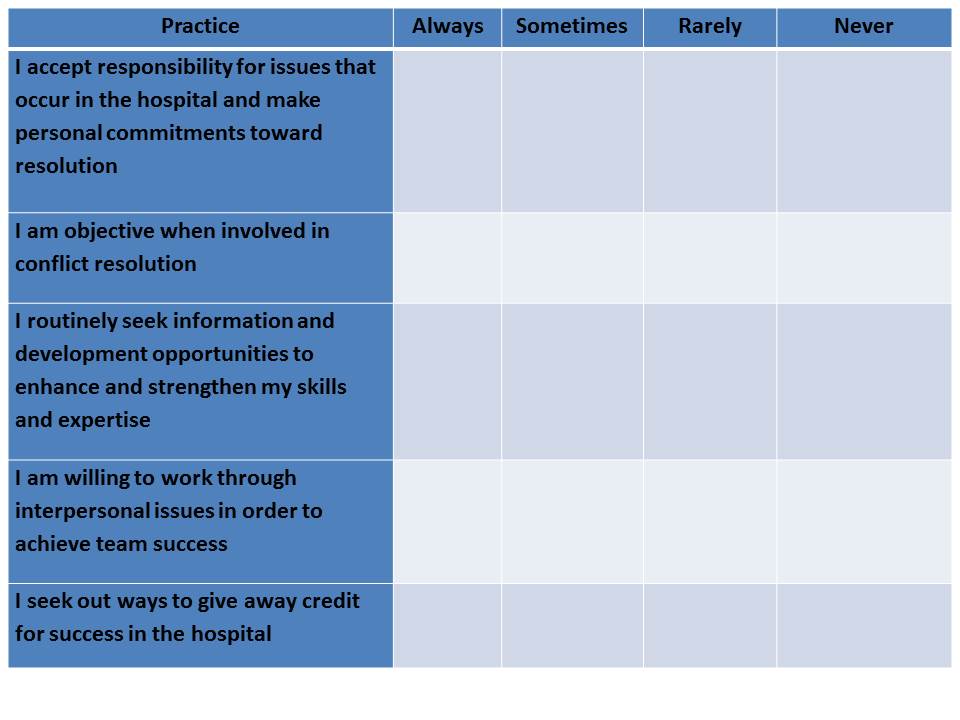
If you answered “Rarely” or “Never” to any of these statements, maybe it’s time to consider a different approach to leadership. Make a commitment to continually ‘check-in’ on your style or approach, with a goal of improving your relationships, interactions, and outcomes. Partner with your manager, or a trusted member of your OPO, to help you grow and develop in your leadership style. Hold yourself personally accountable to fine-tune your ‘principle-centered leadership’ style.
Gweneth D. O’Shaughnessy is Vice President of Hospital Services at Gift of Life Donor Program in Philadelphia, PA
SBAR (Situation – Background – Assessment – Recommendation), is a model of communication commonly used in healthcare today. SBAR was originally developed by the U.S. Navy as a communication technique that could be used on nuclear submarines. In the late 1990s, Safer Healthcare, an organization that focuses on the delivery of specialized products and services supporting the development and sustainability of high reliability organizations (HRO) within the healthcare industry, helped bring this communication model into the healthcare setting. Since that time, SBAR has been adopted by hospitals and care facilities around the world as a simple yet effective way to standardize communication between care givers.
To bring context to SBAR, users should consider the following framework:
Situation Take 5-10 Seconds to Explain
Background Provide Context and Data
Assessment Describe the Specific Problem/Situation
Recommendation Explain What You Want to Do About it and When
If you’re asking yourself, “Why SBAR?” I offer the following:
- It’s the Joint Commission’s stated industry best practice for standardized communication (primarily spoken) in healthcare for effortlessly structuring critical information;
- It promotes quality, patient safety and high reliability because it helps individuals communicate with each other with a shared set of expectations;
- Staff and physicians use SBAR to share patient information in a clear, complete, concise and structured format, improving communication efficiency and accuracy.
How Does SBAR Translate to Organ Procurement Organization (OPO) Professionals?
It can be used in a “Team Huddle” scenario (spoken by the OPO Transplant Coordinator).
| Situation | “The patient has satisfied death by neurologic criteria and has been pronounced dead by Dr. Smith. The patient is medically suitable to donate organs and tissues.” |
| Background | “This patient was a victim of an MVC. Upon meeting clinical triggers, Sue, the bedside RN, referred this patient as a potential donor. The family has now gathered at the bedside to say their good-byes.” |
| Assessment | “Since it appears that the family understands their loved one has died, we now need to formulate a plan for providing the family with their donation opportunity.” |
| Recommendation | “I suggest that we determine which member of the care team has established a trusting relationship with the family and encourage him or her to introduce me and remain present to support the family during the donation conversation. How does this sound?” |
It can be used in a Physician Meeting (spoken by the OPO Hospital Development Coordinator).
| Situation | “We were called to evaluate one of your patients last week as a potential organ donor. The patient’s heart, lungs, liver and kidneys were all successfully transplanted. I wanted to thank you for all that you did to help make this happen.” |
| Background | “It sounds like the family initially really struggled to understand that their loved one had died. Two of your residents spent an extensive amount of time with them.” |
| Assessment | “After talking with your residents about their experience, I think that they are uncomfortable talking to families about death by neurologic criteria.” |
| Recommendation | “I’d like to provide all of your residents with training on how to explain death by neurologic criteria to families. We can customize it to meet whatever time constraints may exist. What do you think?” |
When the organ donation process goes well, it is usually due to collaboration and communication. Similarly, when it doesn’t go well, it’s largely due to breakdowns in these two areas. In hospitals and critical care areas in particular, optimizing our communication is essential. Getting and keeping members of the care team engaged also requires us to evaluate how we are communicating.
- Can we say more with less?
- Are you receiving non-verbal indicators that the listener is busy, disinterested, or in a rush?
- Are you listening for short answers like “yes” or “no” that are potential signs that you provide “Just the Facts Jack”?
- Is the person that you’re attempting to engage asking questions in return?
- Do they seem curious?
- Do they actually sit down to talk with you?
If they appear to have time for a more lengthy conversation then, by all means, take full advantage of that and enjoy the interaction! If they’re not, SBAR is probably the way to go. I strongly recommend that you incorporate this communication model into your approach just once and see how it works.
For additional SBAR information and resources, please visit:
http://www.ihi.org/resources/Pages/Tools/sbartoolkit.aspx
Gweneth D. O’Shaughnessy is Vice President, Hospital Services at Gift of Life Donor Program in Philadelphia, PA



